Abstract
This retrospective cohort study aimed to develop and evaluate a machine-learning algorithm for predicting oliguria, a sign of acute kidney injury (AKI). To this end, electronic health record data from consecutive patients admitted to the intensive care unit (ICU) between 2010 and 2019 were used and oliguria was defined as a urine output of less than 0.5 mL/kg/h. Furthermore, a light-gradient boosting machine was used for model development. Among the 9,241 patients who participated in the study, the proportions of patients with urine output < 0.5 mL/kg/h for 6 h and with AKI during the ICU stay were 27.4% and 30.2%, respectively. The area under the curve (AUC) values provided by the prediction algorithm for the onset of oliguria at 6 h and 72 h using 28 clinically relevant variables were 0.964 (a 95% confidence interval (CI) of 0.963–0.965) and 0.916 (a 95% CI of 0.914–0.918), respectively. The Shapley additive explanation analysis for predicting oliguria at 6 h identified urine values, severity scores, serum creatinine, oxygen partial pressure, fibrinogen/fibrin degradation products, interleukin-6, and peripheral temperature as important variables. Thus, this study demonstrates that a machine-learning algorithm can accurately predict oliguria onset in ICU patients, suggesting the importance of oliguria in the early diagnosis and optimal management of AKI.
Similar content being viewed by others
Introduction
Acute kidney injury (AKI), which is defined as a rapid increase in serum creatinine or decrease in urine output, is one of the leading causes of complications during intensive care unit (ICU) admission, resulting in persistent organ dysfunction and increased mortality1,2,3,4. Although early detection of AKI and prompt intervention can improve the prognosis of critically ill patients, none of the procedures, including close monitoring of vital signs, blood tests, and urine analysis, provides promising solutions. Serum creatinine, which is used to diagnose AKI, has a reduced reliability for the early detection of the pathology5,6,7,8,9.
A recent study showed that oliguria, which is generally defined as a urine output of less than 0.5 mL/kg/h over 6 h, was associated with 90-day mortality irrespective of elevations in serum creatinine levels, exhibiting important diagnostic implications for oliguria in AKI management10. In addition, a prospective observational study showed that continuous monitoring of urine output could identify more patients with AKI earlier than serum creatinine alone11. Therefore, management of AKI with accurate prediction of oliguria may be a promising strategy to understand the complex pathophysiology of critical illnesses better.
With the advancement of artificial intelligence, a substantial number of prediction models using machine-learning algorithms have demonstrated high accuracy in predicting mortality and clinical outcomes in ICU patients, including the detection of AKI12,13,14. In terms of oliguria, a previous study reported a machine-learning approach for predicting urine output in patients with sepsis after fluid administration15. However, the accuracy of a machine-learning model in predicting oliguria in a general ICU setting remains underexplored.
Therefore, we hypothesized that a machine-learning model could predict the onset of oliguria in patients admitted to an ICU. This study aimed to develop a machine-learning algorithm for predicting oliguria in patients at 6 and 72 h, from an arbitrary period, during their ICU stay and to evaluate the accuracy of the developed algorithm using a large database from a single-center surgical/medical mixed ICU.
Results
Characteristics of the cohort
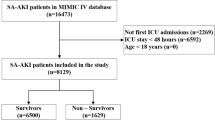
Of the 14,105 patients screened, 4,745 patients without documented body weight and 119 patients on maintenance dialysis were excluded; therefore, only 9,241 patients were included in the study (Supplementary File: Fig. S1). No significant differences were observed between the training and test data. In the entire cohort, the proportions of patients with urine output < 0.5 mL/kg/h for 6 h and with AKI during their ICU stay were 27.4% and 30.2%, respectively (Table 1).
Selection of variables
We used hourly variables and baseline information to develop a sequential machine-learning model to predict oliguria (Fig. 1). From 1,018 variables, 28 variables were selected from a clinical perspective and included in the reduced dataset (Supplementary File: Table S1). Using the light-gradient boosting machine (LightGBM) classifier, we compared the accuracies of the models using all selected variables (Fig. 2). Although the area under the curve (AUC) values for predicting oliguria were comparable between the two methods, the computation time was much longer for the 1,018-variable dataset (56.3 s) than for the 28-variable dataset (7.5 s). The top 50 important variables in the 1,018-variable dataset overlapped with approximately 40% of the selected variables (Supplementary File: Fig. S2). To improve the efficiency and comparative accuracy of the algorithm, we used the 28-variable dataset for further analysis.
Schematic of the sequential machine-learning model for predicting oliguria. The sequential machine-learning model to predict oliguria occurrence at 6 h was developed using hourly variables and baseline information obtained during the ICU stay. The input features were updated to include a 1-h window of the previous values for the physiological parameters, blood tests, and medications. In terms of laboratory tests, the most recent variables were used. ICU intensive care unit.
Sequential accuracy of the machine-learning algorithm for predicting oliguria in the intensive care unit. The line plot depicts the sequential changes in the AUC with the given time for the prediction algorithm for the selected variables (blue) and all variables (yellow). Additionally, the 95% confidence intervals of AUC are shown. AUC area under the curve.
Prediction of oliguria
The AUC of the model to predict oliguria at 6 h using the selected variables was 0.964 (with a 95% confidence interval [CI] of 0.963–0.965). To verify the accuracy of the model, a fivefold cross-validation was implemented with an AUC of 0.920 (95% CI 0.918–0.922). The following Shapley additive explanation (SHAP) values are important variables for predicting oliguria at 6 h: the urine values, sequential organ failure assessment (SOFA) score, serum creatinine, oxygen partial pressure (pO2), fibrinogen/fibrin degradation products (FDP), interleukin (IL)-6, peripheral temperature, creatinine kinase, and total bilirubin (Fig. 3A). The SHAP individual force plots (Fig. 3B,C) show the SHAP values for two patients with and without oliguria. In the first patient, a greater urine volume decreased the probability of oliguria occurrence, whereas the elevation of lactate dehydrogenase (LDH) and FDP increased the probability of oliguria (Fig. 3B). Consequently, the model predicted a lower probability of oliguria occurrence at 6 h. In the second patient, a lower urine volume and higher acute physiology and chronic health evaluation (APACHE) II increased the probability of oliguria occurrence, whereas normal levels of LDH, uric acid (UA), and IL-6 decreased the probability of oliguria. Based on this information, the model predicted an increased risk of oliguria at 6 h (Fig. 3C). The prediction model for the onset of oliguria at 72 h still showed high accuracy (AUC of 0.916 [95% CI 0.914–0.918]). The important variables for predicting oliguria at 72 h based on the SHAP values overlapped with those at 6 h except for urea nitrogen and platelets (Supplementary File: Fig. S3). After analyzing the same dataset using the different computer setting as a sensitivity analysis, we obtained the same results as the primary analysis.
SHAP values of the machine-learning algorithm for predicting oliguria in the intensive care unit. (A) The effect of the features on the output of the model was manifested as the SHAP value. The features are placed in a descending order of importance. The correlation between the feature value and SHAP value reveals the beneficial or adverse impact of the predictor. The magnitude of the value is represented by the red (high) or blue (low) graphs. (B), (C) SHAP individual force plots illustrate the responsible features at scale with a color bar that encompasses the feature contribution to the onset of oliguria in individual cases. Two examples of patients presenting with a high probability of non-oliguria (B) or oliguria (C) are shown. SHAP Shapley additive explanations, SOFA sequential organ failure assessment, pO2 oxygen partial pressure, FDP fibrinogen degradation products, LDH lactate dehydrogenase, APACHE acute physiology and chronic health evaluation, PT-PER prothrombin time; UA uremic acid, APTT activated partial thromboplastin time, Lac lactate.
Subgroup analyses
Next, we analyzed the accuracy of the models in predicting the onset of oliguria at 6 h according to sex, age (≤ 65 and > 66 years), and furosemide administration (Fig. 4A). In this context, the male group was more accurate (AUC = 0.965 [95% CI 0.964–0.967]) than the female group (AUC = 0.946 [95% CI 0.943–0.949]; mean absolute error [MAE] = 0.026). In the age comparison, there was a relatively small difference (MAE = 0.006) between the group younger than 65 years old (AUC = 0.958 [95% CI, 0.958–0.959]) and the group older than 66 years (AUC = 0.962 [95% CI, 0.960–0.964]) (Fig. 4B). Finally, the accuracy of the prediction model was higher for the non-furosemide group (AUC = 0.966 [95% CI 0.964–0.967]) than for the furosemide group (AUC = 0.953 [95% CI 0.951–0.955]), with a greater difference at a later prediction time point (MAE = 0.050) (Fig. 4C).
Subgroup analyses of prediction algorithms for the onset of oliguria in the intensive care unit. The line plot depicts the sequential changes in the area under the curve (AUC) for a given time for the prediction algorithm in the categories of (A) sex, (B) age, and (C) furosemide administration. Differences in the curves of the AUC plots between the two groups were examined using the mean absolute error (MAE) calculated from the averages of the summed absolute values of the differences in AUCs from 6 to 72 h. The MAE values for sex, age, and furosemide administration were 0.026, 0.006, and 0.050, respectively. Moreover, the 95% confidence intervals of the AUC are shown.
Discussion
This study developed a machine-learning model with a high AUC (> 0.96) for predicting the onset of oliguria at 6 h in critically ill patients. Among the 28 clinically relevant variables used for the prediction model, urine values, the SOFA score, serum creatinine, pO2, FDP, IL-6, and peripheral temperature were listed as important variables.
Over the past decade, machine learning algorithms for predicting oliguria in critically ill patients have been underexplored, despite oliguria being one of the key components of AKI that leads to increased mortality in such patients1,16,17,18. Although several studies have repeatedly verified the precision of a machine-learning model to predict AKI in critically ill patients with an AUC range of 0.74 to 0.9319,20,21,22,23,24,25,26, only one study reported a machine-learning approach to predict oliguria for the next 4 h in patients with sepsis after fluid resuscitation using 47 clinical values, with an AUC of 0.8615. Our machine-learning model exhibited a high AUC (> 0.90) for predicting oliguria in critically ill patients between 6 and 72 h. The high accuracy of our model and its capability to predict oliguria over longer periods and fact that the AUC remained the same even after reducing the variables in the model development are a testament to the novel contributions of this study. This high accuracy may be attributed to the large sample size of > 10,000 patients, resulting in abundant training data. In addition, our method of predicting the onset of oliguria from an arbitrary time may have improved the accuracy by increasing the number of training datasets. Although we built the model based on 28 clinically relevant variables, its high overlap with the top-listed variables in the 1,018-value dataset would support the plausibility of using the selected variables for the prediction model. Because oliguria could identify more patients with AKI earlier than serum creatinine alone and is associated with poor outcomes in critically ill patients, our model would be useful for the early detection of patients with AKI and for improving the prognosis of the population through better management and early intervention10,11,27,28.
The SHAP analysis identified urine values, the SOFA score, serum creatinine, pO2, FDP, IL-6, and peripheral temperature as significant predictors of oliguria. Previous studies using SHAP values identified significant factors that increased the risk of ICU-acquired AKI, including a higher body mass index on admission, the presence of chronic kidney disease, congestive heart failure, coagulation and bleeding disorders, and cardiac arrhythmias, in addition to renal function represented by an elevation in blood urea nitrogen or serum creatinine, but not IL-619,24. Because IL-6 is one of the representative cytokines induced by overwhelming systemic inflammation, several studies have reported the significance of blood IL-6 levels for early detection of multiple organ dysfunction29,30,31. The high weight of IL-6 in the development of the predictive model verified the essential role of this cytokine in the progression of organ dysfunction. IL-6 gained wide recognition in the cytokine storm associated with COVID-19 and can now be measured using rapid kits using immunoassays. Moreover, it has emergency approval in the United States32. In a previous study investigating the association between AKI and oliguria in critically ill patients, the SOFA score was higher in patients with oliguria than in those without oliguria in the AKI cohort33. In addition, a multicenter study identified the APACHE II score as a predictor in patients with acute renal failure, requiring dialysis34. These findings support our hypothesis that severity scores play an important role in the early detection of oliguria35. In summary, these important variables can provide insights into the complex pathophysiology of AKI.
In the subgroup analyses, the accuracy of the model in the female and furosemide groups decreased over time compared with that in the other groups, with relatively high accuracy (AUC = 0.86) even at 72 h after the time of observation. A previous study showed that males developed AKI in the ICU more frequently than females due to the protective function of estrogen, which includes proliferative and anti-apoptotic effects on proximal tubular cells. Therefore, physiological differences between the sexes may have affected the accuracy of the model36,37. Additionally, the administration of furosemide, which is arbitrarily timed by a physician, has a direct effect on urine output; therefore, it is conceivable that this subjective intervention could bias the accuracy of the model.
However, this study had the following limitations. First, this retrospective single-center study model may cause uncertainty when applied to different settings although we confirmed the accuracy of the cross-validation methods. Therefore, a prospective study in a different setting is required for future clinical applications. Second, we reduced the number of variables in this study from a clinical perspective; however, we may have missed important variables that affect prediction accuracy. Third, the SHAP analysis included both plausible and uninterpretable variables to predict outcomes. A mechanistic study investigating the significance of these uninterpretable values may reveal their role in the onset of oliguria and AKI. Future research should include an external validation through multicenter studies to verify the prediction accuracy. A prospective investigation is also warranted to evaluate the effects of model application on clinical outcomes.
In conclusion, this study demonstrated that a machine-learning model could predict the onset of oliguria in critically ill patients with high accuracy. Future investigations can focus on validating the accuracy of the prediction model for the early detection of AKI in patients.
Methods
Subjects
This retrospective cohort study used the electronic health record data of consecutive patients admitted to the ICU at Chiba University Hospital, Japan, from November 2010 to March 2019. The annual number of patients admitted to the 22-bed surgical/medical ICU ranged from 1,541 to 1,832. We excluded patients on maintenance dialysis and those without a documented body weight. This study was approved by the Ethical Review Board of Chiba University Graduate School of Medicine (approval number: 3380) in accordance with the Declaration of Helsinki. The Ethical Review Board of Chiba University Graduate School of Medicine waived the requirement for written informed consent in accordance with the Ethical Guidelines for Medical and Health Research Involving Human Subjects in Japan.
Definition of oliguria and AKI
We defined oliguria as urine output of less than 0.5 mL/kg/h according to the Kidney Disease: Improving Global Outcomes stage I criteria. AKI was diagnosed based on an increase in serum creatinine level of at least 0.3 mg/dL from the baseline or oliguria38.
Data collection
Patient records from the ICU data system contained 1,031 input variables, including (A) physiological measurements acquired every minute (heart rate, blood pressure, respiratory rate, peripheral oxygen saturation, and body temperature), (B) blood tests (complete blood count, biochemistry, coagulation, and blood gas analysis), (C) name and dosage of medications, (D) type and amount of blood transfusion, (E) patient observation record, and (F) patient care record. The minute-by-minute time-series tables were aggregated into hourly time-series tables. In the process of aggregating the tables, the median value was used for physiological measurements and the blood test values were obtained from the most recent test. For patient excretion values, urine and stool volumes were calculated as one-hour sums. The following six calculated variables were added to the dataset: hourly intake, hourly output, hourly total balance, hourly urine volume (mL/kg), oliguria (urine volume of less than 0.5 mL/kg/h), and oliguria for six consecutive hours. A total of 222 background information variables, including age, sex, and admission diagnosis, were also added to the dataset. Consequently, the dataset contained 1,127 variables. We treated the missing values as a separate group or excluded them from the analysis. To remove potential collinearity values, we performed a multicollinearity test and analyzed the data without these values.
Machine learning algorithms and statistical analyses
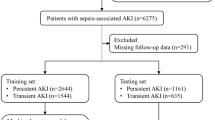
The dataset was randomly divided: 80% for training and 20% for testing. We developed a sequential machine-learning model to predict oliguria at any given time during the ICU stay using hourly variables and baseline information (Fig. 1). For the values that were not continuously obtained, we used the most recent ones for the model development. The input variables were updated to encompass a 1-h window of the preceding values for the physiological measurements, blood tests, and medications. The primary and secondary outcome variables were oliguria at 6 and 72 h after an arbitrary time point from ICU admission to discharge, respectively. Accordingly, we used variables recorded until 6 or 72 h before ICU discharge corresponding to each outcome variable. The outcome variable was not incorporated as a predictor in the final model. After constructing the algorithm with the training data, the model predictions were validated using the test data. We validated the model performance with a fivefold cross validation. To ensure that the estimated model probabilities aligned with the actual probabilities of oliguria occurrence, we plotted the calibration curve of the model. The curve indicated that our model was well calibrated (Supplementary File 1: Fig. S4).
We selected four representative machine learning classifiers: LightGBM, category boosting (CatBoost), random forest, and extreme gradient boosting (XGboost). Before developing the prediction model, we compared the computational performances and model accuracies using the four classifiers (Supplementary File 1: Table S2). To develop the machine learning algorithm, we used a cloud computer (Google Collaboratory memory 25 GB) to evaluate the accuracy of the model. The AUC values based on the receiver operating calibrating curves, sensitivity, specificity, and F1 score were calculated. Among the machine learning classifiers, LightGBM showed the best computation speed and AUC and the second-best F1 score with a marginal difference from XGboost (XGboost 0.899, LightGBM 0.896). Based on these results, we decided to use LightGBM for the analysis in this study. After developing a prediction model with all the variables, we reduced the number of variables for prediction by selecting clinically relevant variables (Supplementary File: Table S2). Subsequently, we compared the performances of the LightGBM model using the selected variables and all the variables. As a sensitivity analysis, we re-analyzed the data using a different computer environment, Amazon Web Service Sagemaker. The computer settings included the following: image: Data Science 3.0, kernel: python 3, and instance type: ml.t3.medium (memory 64 GB).
To evaluate the important variables contributing to building the prediction model, we used the SHAP value. The SHAP value indicates the impact of each feature on the model output, with higher interpretability in machine learning models. We expressed the SHAP value as an absolute number with a positive or negative association between the variable and outcome. SHAP individual force plots showed several features at scale with a color bar that indicated the feature contribution to the onset of oliguria in individual instances, enhancing the interpretability regarding the connection between traits and the occurrence of oliguria. For the subgroup analyses, we compared the accuracies of the models in predicting oliguria based on sex, age (≤ 65 or > 66 years), and furosemide administration. To quantify the differences in the AUC plots of the two groups, the absolute values of the differences in the AUCs of each group from 6 to 72 h were summed and averaged to obtain the MAE.
Data were expressed as medians with interquartile ranges for continuous values and as absolute numbers and percentages for categorical values. A P value < 0.05 was considered as statistically significant. The main Python packages used in the analysis to create the machine learning algorithms were Python 3.10.11, pandas 1.5.3, numpy 1.22.4, matplotlib 3.7.1, scikit-learn 1.2.2, XGboost 1.7.2, lightgbm 2.2.3, catboost 1.1.1, and shap 0.41.0.
Data availability
The datasets used and analyzed in this study will be available from the corresponding author upon reasonable request.
References
Wang, H. E., Muntner, P., Chertow, G. M. & Warnock, D. G. Acute kidney injury and mortality in hospitalized patients. Am. J. Nephrol. 35, 349–355. https://doi.org/10.1159/000337487 (2012).
Buttner, S. et al. Incidence, risk factors, and outcome of acute kidney injury in neurocritical care. J. Intensive Care Med. 35, 338–346. https://doi.org/10.1177/0885066617748596 (2020).
Ronco, C., Bellomo, R. & Kellum, J. A. Acute kidney injury. Lancet 394, 1949–1964. https://doi.org/10.1016/S0140-6736(19)32563-2 (2019).
Khwaja, A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin. Pract. 120, c179-184. https://doi.org/10.1159/000339789 (2012).
Taguchi, K. et al. Cyclin G1 induces maladaptive proximal tubule cell dedifferentiation and renal fibrosis through CDK5 activation. J. Clin. Invest. https://doi.org/10.1172/JCI158096 (2022).
Pan, H. C. et al. Comparative accuracy of biomarkers for the prediction of hospital-acquired acute kidney injury: A systematic review and meta-analysis. Crit Care 26, 349. https://doi.org/10.1186/s13054-022-04223-6 (2022).
Porrini, E. et al. Estimated GFR: Time for a critical appraisal. Nat. Rev. Nephrol. 15, 177–190. https://doi.org/10.1038/s41581-018-0080-9 (2019).
Luft, F. C. Biomarkers and predicting acute kidney injury. Acta Physiol. 231, e13479. https://doi.org/10.1111/apha.13479 (2021).
Van Acker, P. et al. Risk prediction models for acute kidney injury in adults: An overview of systematic reviews. PLoS One 16, e0248899. https://doi.org/10.1371/journal.pone.0248899 (2021).
Bianchi, N. A. et al. Association of oliguria with acute kidney injury diagnosis, severity assessment, and mortality among patients with critical illness. JAMA Netw. Open 4, e2133094. https://doi.org/10.1001/jamanetworkopen.2021.33094 (2021).
Willner, D. et al. Early identification of acute kidney injury in the ICU with real-time urine output monitoring: A clinical investigation. BMC Nephrol 22, 293. https://doi.org/10.1186/s12882-021-02485-w (2021).
Shillan, D., Sterne, J. A. C., Champneys, A. & Gibbison, B. Use of machine learning to analyse routinely collected intensive care unit data: A systematic review. Crit. Care 23, 284. https://doi.org/10.1186/s13054-019-2564-9 (2019).
Iwase, S. et al. Prediction algorithm for ICU mortality and length of stay using machine learning. Sci. Rep. 12, 12912. https://doi.org/10.1038/s41598-022-17091-5 (2022).
Tomasev, N. et al. A clinically applicable approach to continuous prediction of future acute kidney injury. Nature 572, 116–119. https://doi.org/10.1038/s41586-019-1390-1 (2019).
Lin, P. C. et al. A machine learning approach for predicting urine output after fluid administration. Comput. Methods Programs Biomed. 177, 155–159. https://doi.org/10.1016/j.cmpb.2019.05.009 (2019).
Zeng, X., McMahon, G. M., Brunelli, S. M., Bates, D. W. & Waikar, S. S. Incidence, outcomes, and comparisons across definitions of AKI in hospitalized individuals. Clin. J. Am. Soc. Nephrol. 9, 12–20. https://doi.org/10.2215/CJN.02730313 (2014).
Bellomo, R. et al. Acute kidney injury in sepsis. Intensive Care Med. 43, 816–828. https://doi.org/10.1007/s00134-017-4755-7 (2017).
Zhang, Z., Ho, K. M. & Hong, Y. Machine learning for the prediction of volume responsiveness in patients with oliguric acute kidney injury in critical care. Crit. Care 23, 112. https://doi.org/10.1186/s13054-019-2411-z (2019).
Shawwa, K. et al. Predicting acute kidney injury in critically ill patients using comorbid conditions utilizing machine learning. Clin. Kidney J. 14, 1428–1435. https://doi.org/10.1093/ckj/sfaa145 (2021).
Zimmerman, L. P. et al. Early prediction of acute kidney injury following ICU admission using a multivariate panel of physiological measurements. BMC Med. Inform. Decis Mak. 19, 16. https://doi.org/10.1186/s12911-019-0733-z (2019).
Zhang, X. et al. Machine learning for the prediction of acute kidney injury in critical care patients with acute cerebrovascular disease. Ren Fail 44, 43–53. https://doi.org/10.1080/0886022X.2022.2036619 (2022).
Alfieri, F. et al. A deep-learning model to continuously predict severe acute kidney injury based on urine output changes in critically ill patients. J. Nephrol. 34, 1875–1886. https://doi.org/10.1007/s40620-021-01046-6 (2021).
Le, S. et al. Convolutional neural network model for intensive care unit acute kidney injury prediction. Kidney Int. Rep. 6, 1289–1298. https://doi.org/10.1016/j.ekir.2021.02.031 (2021).
Wei, C., Zhang, L., Feng, Y., Ma, A. & Kang, Y. Machine learning model for predicting acute kidney injury progression in critically ill patients. BMC Med. Inform. Decis Mak. 22, 17. https://doi.org/10.1186/s12911-021-01740-2 (2022).
Qian, Q., Wu, J., Wang, J., Sun, H. & Yang, L. Prediction models for aki in icu: A comparative study. Int. J. Gen. Med. 14, 623–632. https://doi.org/10.2147/IJGM.S289671 (2021).
Liang, Q. et al. Severe acute kidney injury predicting model based on transcontinental databases: A single-centre prospective study. BMJ Open 12, e054092. https://doi.org/10.1136/bmjopen-2021-054092 (2022).
Heffernan, A. J. et al. Association between urine output and mortality in critically ill patients: A machine learning approach. Crit. Care Med. 50, e263–e271. https://doi.org/10.1097/CCM.0000000000005310 (2022).
Rank, N. et al. Deep-learning-based real-time prediction of acute kidney injury outperforms human predictive performance. NPJ Digit. Med. 3, 139. https://doi.org/10.1038/s41746-020-00346-8 (2020).
Shimazui, T. et al. Blood interleukin-6 levels predict multiple organ dysfunction in critically ill patients. Shock 55, 790–795. https://doi.org/10.1097/SHK.0000000000001678 (2021).
Shimazui, T., Matsumura, Y., Nakada, T. A. & Oda, S. Serum levels of interleukin-6 may predict organ dysfunction earlier than SOFA score. Acute Med. Surg. 4, 255–261. https://doi.org/10.1002/ams2.263 (2017).
Oda, S. et al. Sequential measurement of IL-6 blood levels in patients with systemic inflammatory response syndrome (SIRS)/sepsis. Cytokine 29, 169–175. https://doi.org/10.1016/j.cyto.2004.10.010 (2005).
Mehta, P. et al. COVID-19: Consider cytokine storm syndromes and immunosuppression. Lancet 395, 1033–1034. https://doi.org/10.1016/S0140-6736(20)30628-0 (2020).
Vaara, S. T. et al. Association of oliguria with the development of acute kidney injury in the critically ill. Kidney Int. 89, 200–208. https://doi.org/10.1016/j.kint.2015.12.007 (2016).
Parker, R. A. et al. Prognosis of patients with acute renal failure requiring dialysis: Results of a multicenter study. Am. J. Kidney Dis. 32, 432–443. https://doi.org/10.1053/ajkd.1998.v32.pm9740160 (1998).
Lee, D. W., Faubel, S. & Edelstein, C. L. Cytokines in acute kidney injury (AKI). Clin. Nephrol. 76, 165–173. https://doi.org/10.5414/cn106921 (2011).
Guzel, C. et al. The effect of gender on acute kidney injury developing in the intensive care unit. Hippokratia 23, 126–130 (2019).
Neugarten, J. & Golestaneh, L. Gender and the prevalence and progression of renal disease. Adv. Chronic Kidney Dis. 20, 390–395. https://doi.org/10.1053/j.ackd.2013.05.004 (2013).
Section 2: AKI Definition. Kidney Int Suppl (2011) 2, 19–36, doi:https://doi.org/10.1038/kisup.2011.32 (2012).
Acknowledgements
We would like to thank Honyaku Center Inc. for English language editing.
Author information
Authors and Affiliations
Contributions
Y.Y., T.O., J.Y., N.T., and T.N. were responsible for the study concept and design, statistical analysis, interpretation of the data, drafting of the manuscript, and critical revision of the manuscript for important intellectual content. Y.Y. and J.Y. performed the computing process to extract the necessary data, statistical analysis, and data interpretation. All the other authors interpreted the data and critically revised the manuscript for important intellectual content. All the authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
TN is the CEO of Smart119 Inc. and owns stock. YY also owns stock in Smart119, Inc. Smart119 Inc. had no role in the study design, data analysis, or manuscript preparation. The other authors have no competing interest to declare.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yamao, Y., Oami, T., Yamabe, J. et al. Machine-learning model for predicting oliguria in critically ill patients. Sci Rep 14, 1054 (2024). https://doi.org/10.1038/s41598-024-51476-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-51476-y